- Physicians
- Clinics
- TCM
- Western GP
-
Fees
-
Deals & Privileges
- About & Resources
- Contact Us
Persistent Cough After Respiratory Infections
Recently, many people have reported lingering throat itch and cough after recovering from colds, flu, or COVID-19. While other symptoms have subsided, they are left with a dry cough or stubborn phlegm that's hard to expel.
A major reason for this is the depletion of body fluids (yin deficiency) caused by the battle between pathogens and the immune system during the infection.
Some dismiss throat issues as minor and rely solely on heat-clearing or anti-inflammatory drugs, unaware that such neglect can worsen the condition and even affect the ears and nose.

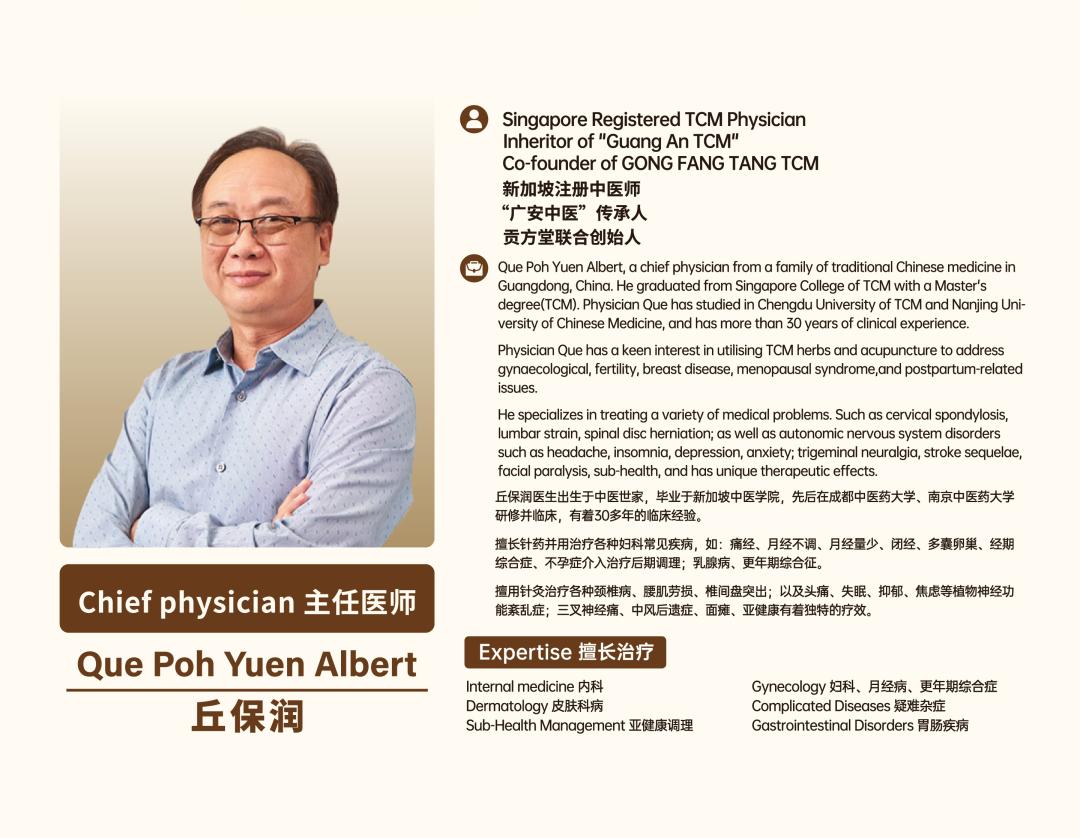
TCM Expert Que Poh Yuen Albert from Singapore's Gong Fang Tang TCM Explains the Causes
According to Dr. Que Poh Yuen Albert, a TCM specialist at Singapore’s Gong Fang Tang TCM, these symptoms arise due to two main factors:
Viral Damage to Respiratory Mucosa
Colds are often caused by viral infections, which attack the respiratory tract, damaging the mucosal lining and leading to symptoms like dryness and itchiness in the throat.
Impaired Lung Function in TCM Terms
A cold can disrupt lung qi dispersion (肺气不宣) and impair the lung’s ability to clear and descend (肺失清肃), triggering coughing.
Difficulty expelling phlegm may result from thick, sticky phlegm or insufficient lung qi, making it hard to cough up effectively.
Many experience soreness, itching, a burning sensation, or the feeling of something stuck in the throat, which is extremely uncomfortable.
In TCM theory, these issues stem from insufficient body fluids (津液), which belong to the yin category. When yin fluids are depleted, they fail to properly moisten the throat.
To resolve this, the primary approach is to:
Nourish yin and moisten dryness (滋阴润燥)
Supplement with heat-clearing and fire-purging herbs
This combination effectively addresses the problem.

Preferred TCM Herbs for Treatment
Therefore, certain Chinese herbs that nourish yin, moisten the lungs, clear heat and toxins, soothe the throat, suppress coughs, relieve itching, and even cool blood and activate circulation become the primary choice for treatment.
For example, the following formula is particularly suitable:
Ingredients:
Xuan Shen (Scrophularia root) – 9g
Mai Dong (Ophiopogon tuber) – 9g
Sheng Gan Cao (Raw licorice root) – 6g
Jie Geng (Platycodon root) – 9g
Indications:
Dry, itchy throat due to lung and kidney yin deficiency with deficient fire flaring upward
Dry cough with scanty phlegm, possibly blood-streaked
Dry mouth and tongue, hoarse voice
Effects:
Nourishes yin and clears heat
Moistens the lungs and tonifies the kidneys
Relieves cough and dispels phlegm
Preparation:
Soak the herbs for 15 minutes before decocting for 30 minutes.
If decoction is inconvenient, steep in boiling water as a herbal tea.
For better taste, add a small amount of honey when drinking.
The redness, swelling, dryness, itching, and foreign body sensation in the throat are often attributed to inflammation in Western medicine. In TCM, this condition is called "喉痹 (hou bi)" or "喉闭 (hou bi)", referring to a state of stagnant qi and blood flow, leading to blockage in the throat.
Causes of "Hou Bi":
Exposure to pathogenic heat or toxins
Excessive consumption of spicy, heat-inducing foods, leading to stomach heat rising to the throat
This formula specifically treats "deficient-fire hou bi" caused by:
Lung and kidney yin deficiency
Deficient heat disturbing the upper body
When lung yin is insufficient, the throat loses its nourishment, and deficient fire flares upward, resulting in:
Dryness and itching
Dry cough with little phlegm
Hoarseness
Unlike excess-heat syndromes (requiring heat-clearing, detoxifying, and throat-soothing herbs), deficient-fire hou bi requires:
Tonifying kidney yin
Clearing deficient heat
Commonly used herbs include:
Mai Dong (Ophiopogon)
Xuan Shen (Scrophularia)
Di Huang (Rehmannia)
Niu Xi (Achyranthes root)

Patient: Zhang, female, 63 years old
Chief Complaint: "Recurrent cough persisting for over half a year"
Case Presentation:
The patient developed unexplained coughing, which occurs suddenly without warning, day or night. The cough is loud and accompanied by shortness of breath, with tearing and nasal discharge. Each episode lasts nearly half an hour, with little to no phlegm or only scanty frothy saliva. No fever or chills were observed. Appetite is normal, but sleep is disturbed due to coughing. Bowel and urinary functions remain normal.
Current Symptoms:
Thin physique, fatigued appearance
Red and swollen throat with follicular hyperplasia
Reduced appetite
Normal bowel and urinary function
Poor sleep quality
Tongue: Red with thin, scant coating
Pulse: Thin and rapid
Diagnosis: Cough (肺燥阴虚型, Dry Cough due to Lung Yin Deficiency)
Prescription:
Xuan Shen (Scrophularia root) – 10g
Jie Geng (Platycodon root) – 10g
Mai Dong (Ophiopogon tuber) – 10g
Zhi Gan Cao (Honey-fried licorice root) – 5g
Feng Huang Yi (Eggshell membrane) – 5g
Chan Yi (Cicada molting) – 5g
Pi Pa Ye (Loquat leaf) – 10g
Mu Hu Die (Indian trumpet flower seed) – 5g
Ma Bo (Puffball fungus) – 5g
Fu Ling (Poria cocos) – 15g
Chen Pi (Tangerine peel) – 10g
Dosage & Administration:
4 doses, decocted in water
Take warm after breakfast and dinner
Discontinue all other medications

The patient reported no significant improvement in coughing, but throat itching had resolved. Appetite remained normal, bowel movements were regular, and sleep quality had improved.
Examination Findings:
Reduced throat congestion
Tongue: Pale red with thin white coating
Pulse: Thin
Modified Prescription:
Retained the original formula but:
Mi Zi Wan (Honey-fried Aster root) – 10g
Bei Sha Shen (Glehnia root) – 15g
Removed Ma Bo (Puffball fungus) and Fu Ling (Poria cocos)
Reduced Jie Geng (Platycodon root) to 6g
Added:
Dosage & Administration:
5 doses, decocted in water
Same administration method as before
Follow-up:
The patient reported complete resolution of cough after finishing the prescribed medication.
Disclaimer:
This case is intended to illustrate TCM diagnostic and treatment principles and should not be used as medical guidance. Any herbal use must be individually prescribed by a qualified TCM practitioner.