- Physicians
- Clinics
- TCM
- Western GP
-
Fees
-
Deals & Privileges
- About & Resources
- Contact Us
Menopause marks the transition of a woman's life into old age.
Yet many people think: "I'm still young, menopause is far away for me."
But in reality, certain behaviors may lead to premature amenorrhea (cessation of menstruation).
In modern society, with the acceleration of life pace and environmental changes, early amenorrhea in middle-aged women before the natural menopausal age has become increasingly common.
Modern medicine attributes this mostly to premature ovarian atrophy and failure, which is often difficult to treat.
But our ancestors had solutions!

Menstruation is a routine experience for women, and menstrual disorders are common gynecological issues. However, many are unaware that irregular periods often signal underlying health problems—some of which can significantly impact quality of life.
Amenorrhea is defined as:
Primary amenorrhea: No onset of menstruation by age 16.
Secondary amenorrhea: Cessation of menstruation for over 6 months (or 3+ cycles based on the individual’s normal cycle) in women who previously had regular periods, excluding physiological causes like pregnancy or breastfeeding.
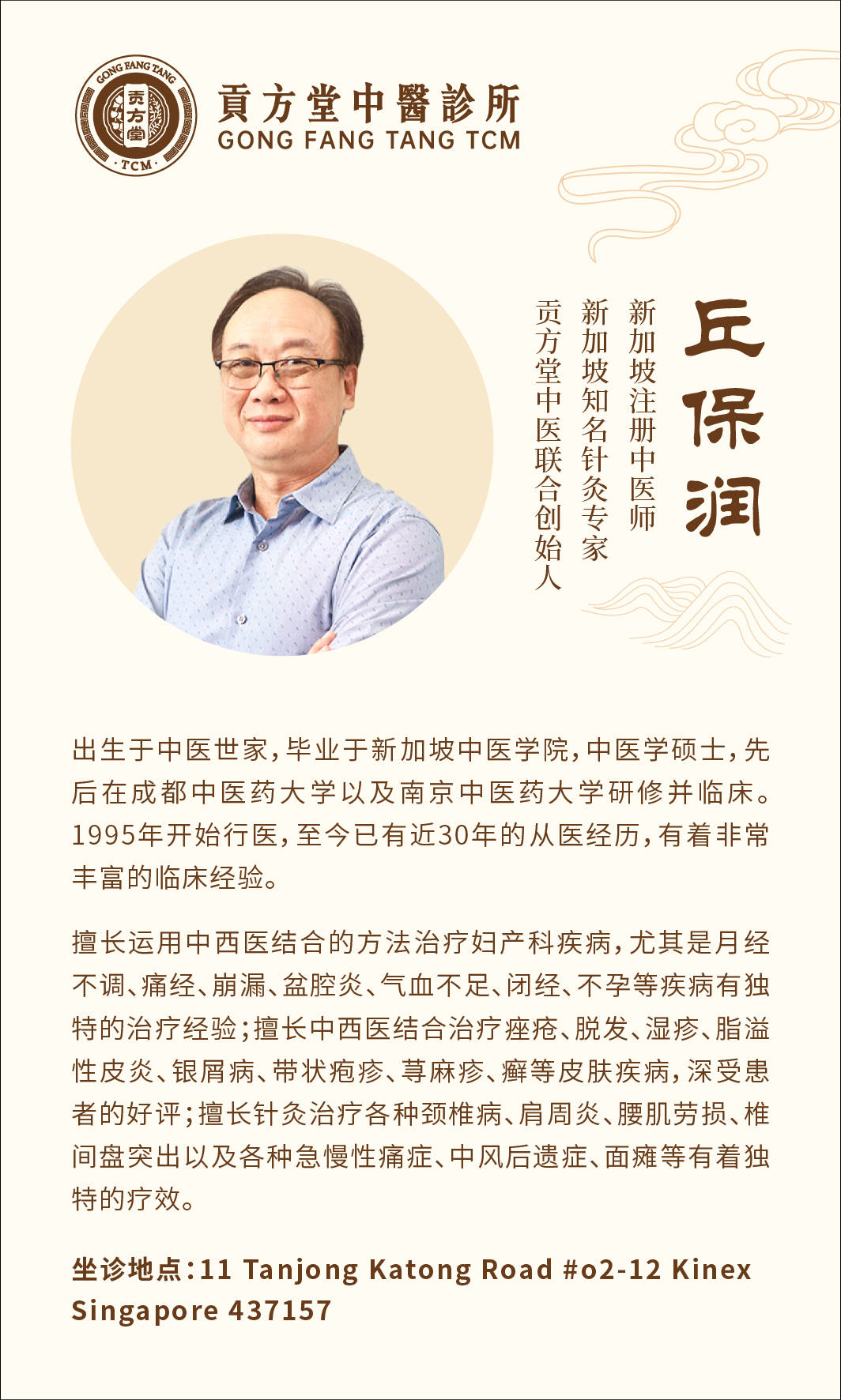
Dr. Que Poh Yuen Albert, a TCM gynecology specialist at Singapore’s Gong Fang Tang Traditional Chinese Medicine, notes that amenorrhea is a frequent yet complex disorder, with some cases posing significant treatment challenges.
Western Medicine Perspective:
Amenorrhea may stem from uterine, ovarian, pituitary, hypothalamic, adrenal, or thyroid dysfunction, and is classified as primary or secondary.
TCM Perspective:
It is categorized into deficiency patterns, excess patterns, or mixed deficiency-excess patterns. Treatment follows these principles:
Deficiency: Tonify and unblock ("supplement to restore flow").
Excess: Purge and unblock ("drain to restore flow").
Mixed patterns: Combine tonification with regulation ("nourish while promoting circulation").
TCM Pathophysiology:
Amenorrhea is closely tied to dysfunction of the zang-fu organs, qi-blood imbalance, and disruption of the Chong and Ren meridians.
Kidney deficiency is the root cause.
Blood stasis is the manifestation.
Thus, the core treatment strategy focuses on kidney tonification, blood-activation, and cycle regulation.

Medical Case Report
Patient: Ms. Pan, female, 40 years old
Chief Complaint:
Previously had regular menstruation until age 40.
Over the past 5 months:
Flushed face
Spontaneous sweating
Heat sensation in palms/soles (五心烦热)
Vaginal dryness
Reduced vaginal discharge
Dry throat and mouth
Delayed periods with scanty flow → complete cessation
Accompanied by:
Ultrasound: Normal uterus and adnexa.
Tongue: Red with scant coating.
Pulse: Thready and rapid.
TCM Diagnosis:
Yin deficiency with blood dryness (阴虚血燥)
Treatment Principle:
Nourish yin, enrich blood → replenish the Chong and Ren meridians.
Prescription: Modified Yiguan Jian (一贯煎) + Zhi Bai Dihuang Tang (知柏地黄汤)
White peony root (白芍) – 12g
Prepared rehmannia (熟地黄) – 12g
Anemarrhena rhizome (知母) – 10g
Phellodendron bark (黄柏) – 10g
Chinese angelica (当归) – 12g
Cornus fruit (山茱萸) – 15g
Moutan bark (牡丹皮) – 10g
Glehnia root (沙参) – 15g
Wolfberry fruit (枸杞子) – 15g
Lycium root bark (地骨皮) – 12g
Ligustrum fruit (女贞子) – 20g
Eclipta herb (旱莲草) – 20g
Prepared turtle shell (炙鳖甲) – 10g
Preparation: Decoct in water, 1 dose daily.
Second Visit:
After 10 doses:
No menstruation yet.
Reduced facial flushing, sweating, and heat sensation.
Vaginal dryness and throat/mouth dryness persisted.
Modified prescription:
Fresh rehmannia (生地黄) – 12g
Prepared tortoise plastron (炙龟板) – 10g
Added:
Continued for 10 more doses.
Third Visit:
Still no menstruation, but all symptoms further improved.
Adjusted regimen:
Take the same formula every other day for 30 doses.
Follow-up: Patient reported return of menstruation after completion, though flow was scanty (lasting 3 days).
Maintenance protocol:
Take 4 doses monthly for 3 months to consolidate effects.
Case Analysis:
This case represents premature ovarian failure with amenorrhea, often accompanied by menopausal-like symptoms.
Clinical patterns typically involve:
Yin deficiency with fire excess (阴虚火旺)
Deficiency of both yin and yang (阴阳俱虚)
Yin deficiency with blood dryness (阴虚血燥)
Treatment strategy:
Focused on nourishing yin and blood.
By replenishing yin-blood and restoring the Chong-Ren meridians, menstrual flow naturally resumed.

In summary, amenorrhea is often linked to factors such as:
Congenital deficiencies
Emotional imbalances
Dietary irregularities or overexertion
Exposure to cold pathogens
Treatment should be tailored to the specific syndrome pattern, including methods such as:
Nourishing the liver and kidneys
Replenishing qi and blood
Regulating qi and activating blood circulation
Resolving phlegm and dampness
Warming the meridians to dispel cold
In modern women, excess-type amenorrhea (e.g., qi stagnation, blood stasis, phlegm-dampness) is more common. Identifying constitutional patterns and targeted therapy is key to effective treatment.
Warning signs requiring medical attention:
Delayed menstruation (≥3 months)
Sudden decrease in menstrual flow
Hot flashes, night sweats
Irritability, insomnia
If these symptoms occur, seek prompt evaluation to prevent premature amenorrhea.